Dialysis 101: What Nursing Home Staff Need to Know
As the number of nursing home residents requiring dialysis increases, it's essential for long-term care staff to have a foundational understanding of dialysis treatments. This knowledge ensures better coordination with dialysis providers and enhances resident care.
Understanding Dialysis
Dialysis is a life-sustaining treatment for individuals with End-Stage Renal Disease (ESRD), where the kidneys can no longer effectively filter waste and excess fluids from the blood. There are two primary types of dialysis:
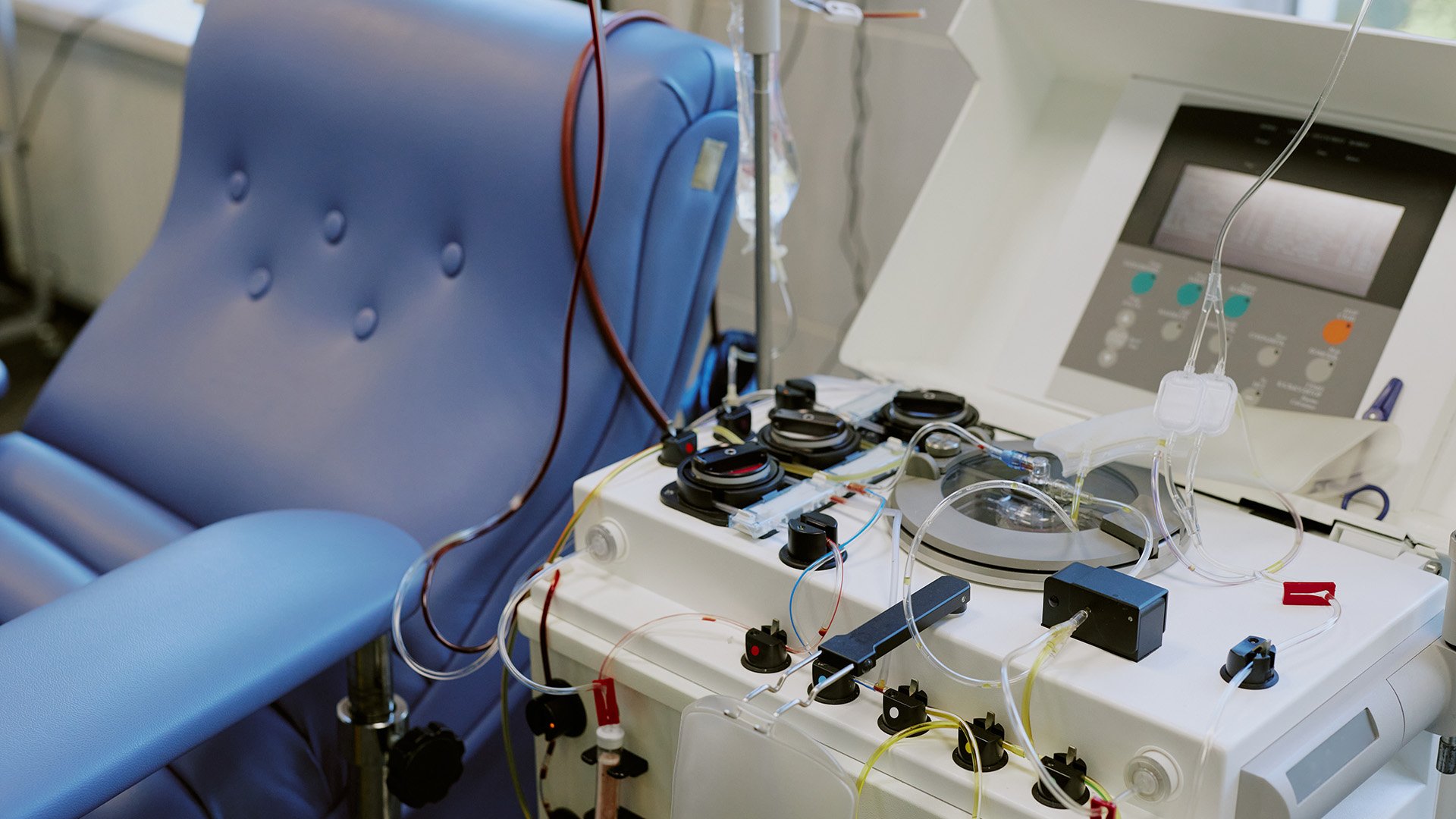
Hemodialysis (HD)
- Process: Blood is drawn from the body, filtered through a dialyzer (artificial kidney), and returned.
- Setting: Typically performed in outpatient dialysis centers three times a week, each session lasting about four hours.
- Access: Requires a vascular access point, such as a fistula, graft, or catheter.
Peritoneal Dialysis (PD)
- Process: A cleansing fluid is introduced into the abdominal cavity, where the peritoneal membrane acts as a filter. After a dwell time, the fluid, now containing waste products, is drained.
- Setting: Often conducted at home, either manually throughout the day (Continuous Ambulatory Peritoneal Dialysis - CAPD) or automatically at night using a machine (Continuous Cycling Peritoneal Dialysis - CCPD).
- Access: Involves a catheter surgically placed into the abdomen.
Key Considerations for Nursing Home Staff
Scheduling and Transportation
Residents undergoing hemodialysis will have fixed treatment schedules. Coordinating transportation to and from dialysis centers is crucial to prevent missed sessions, which can lead to serious health complications.
Monitoring for Complications
Be vigilant for signs of potential complications:
- Infection: Redness, swelling, or discharge at access sites.
- Hypotension: Dizziness or fainting, especially post-dialysis.
- Fluid Overload: Swelling in limbs, shortness of breath.
Promptly report any concerns to the resident's healthcare provider.
Dietary Management
Residents on dialysis often have specific dietary restrictions, including limits on sodium, potassium, phosphorus, and fluid intake. Collaborate with dietitians to ensure meal plans align with these requirements.
Medication Administration
Some medications are administered during dialysis sessions, while others may need dosage adjustments due to reduced kidney function. Maintain clear communication with the dialysis team to ensure accurate medication management.
In-House Dialysis: An Emerging Option
Some nursing homes are exploring the feasibility of providing dialysis on-site. This approach can reduce the physical strain of transportation for residents and allow for more flexible scheduling. Implementing in-house dialysis requires collaboration with certified dialysis providers and adherence to regulatory guidelines.
Subscribe to the Qsource Blog
Get emailed articles, guides, and updates.



